Consider using prednisone as an adjunct therapy for pneumonia, particularly in cases of severe inflammation or exacerbation of underlying lung conditions. Prednisone, a corticosteroid, helps reduce inflammation, thus improving respiratory function and facilitating recovery.
Clinical evidence supports prednisone’s role in managing patients with pneumonia, especially those experiencing significant respiratory distress or those at higher risk for deterioration. It is essential to tailor the dosage based on the severity of the condition and individual patient factors, typically starting with a higher dose and tapering down as needed.
Monitoring for potential side effects, such as hyperglycemia or infection risk, remains critical while on prednisone. Additionally, combining this treatment with antibiotics and supportive care provides a more comprehensive approach to pneumonia management, ensuring a greater chance of recovery and reducing the likelihood of complications.
- Prednisone for Treatment of Pneumonia
- Understanding Pneumonia and Its Causes
- Role of Corticosteroids in Pneumonia Management
- Indications for Use
- Potential Risks and Benefits
- Indications for Prescribing Prednisone in Pneumonia
- Specific Populations for Prednisone Use
- Clinical Considerations
- Dosage Guidelines for Prednisone Use in Pneumonia
- Potential Side Effects and Risks of Prednisone
- Physical Side Effects
- Serious Risks
- Clinical Studies and Evidence Supporting Prednisone Efficacy
- Clinical Trial Data
- Mechanism of Action
Prednisone for Treatment of Pneumonia
Prednisone can be beneficial in certain situations for patients with pneumonia, particularly in those with severe inflammation or obstructive airway difficulties. It is a corticosteroid that reduces inflammation, which can alleviate symptoms and improve respiratory function.
Consider the following guidelines for using prednisone in pneumonia treatment:
- Indications: Use prednisone for patients with severe pneumonia, especially if they have underlying conditions like asthma or COPD.
- Dosing: The typical initial dose may range from 40 mg to 60 mg per day, depending on the severity of symptoms. Tapering the dosage should follow after an improvement.
- Duration: Treatment duration can last from 5 to 10 days, but the specific length should be individualized based on clinical response.
- Monitoring: Regularly assess respiratory function and signs of secondary infections while on prednisone therapy.
It’s critical to weigh the benefits against potential side effects, such as increased susceptibility to infections, gastrointestinal disturbances, or mood changes. Always discuss with a healthcare provider before starting treatment.
Infection control remains a priority. While prednisone can help with inflammation, it should complement antibiotics or other treatments targeting the pneumonia itself rather than replace them. Consistent follow-ups ensure that treatment remains on track and adjustments are made if necessary.
Consider consulting with a specialist if the patient does not show improvement within a few days or if they suffer from recurrent pneumonia cases. These scenarios may require a more comprehensive treatment strategy.
Understanding Pneumonia and Its Causes
Pneumonia is an infection that inflames the air sacs in one or both lungs, leading to difficulty in breathing and chest discomfort. It can be caused by various pathogens, including bacteria, viruses, and fungi. Each type of pneumonia may have different treatment approaches, including the potential use of medications like prednisone for specific cases.
Key causes of pneumonia include:
- Bacterial Infections: Streptococcus pneumoniae is the most common bacterium responsible for pneumonia. This form often occurs after a cold or flu.
- Viral Infections: Influenza virus, respiratory syncytial virus (RSV), and coronaviruses can lead to viral pneumonia, typically affecting younger children and older adults.
- Fungal Infections: Fungi such as Histoplasma and Coccidioides can cause pneumonia, especially in individuals with weakened immune systems.
- Aspiration: Inhalation of food, liquid, or vomit into the lungs may lead to aspiration pneumonia, primarily affecting people with swallowing difficulties.
- Environmental Factors: Exposure to pollutants, chemicals, and allergens may contribute to the risk of developing pneumonia.
Recognizing symptoms of pneumonia is critical for timely treatment. Common signs include:
- Persistent cough, which may produce phlegm
- Fever, chills, and sweating
- Shortness of breath or rapid breathing
- Chest pain that worsens with deep breaths
Consult a healthcare provider if these symptoms arise, as early intervention can significantly impact recovery. Knowing the causes of pneumonia helps in prevention strategies and identifies populations at higher risk, such as children, the elderly, and individuals with certain medical conditions.
Overall, understanding pneumonia’s various causes enables better management and treatment options, including the consideration of appropriate medications like prednisone for specific cases where inflammation plays a significant role.
Role of Corticosteroids in Pneumonia Management
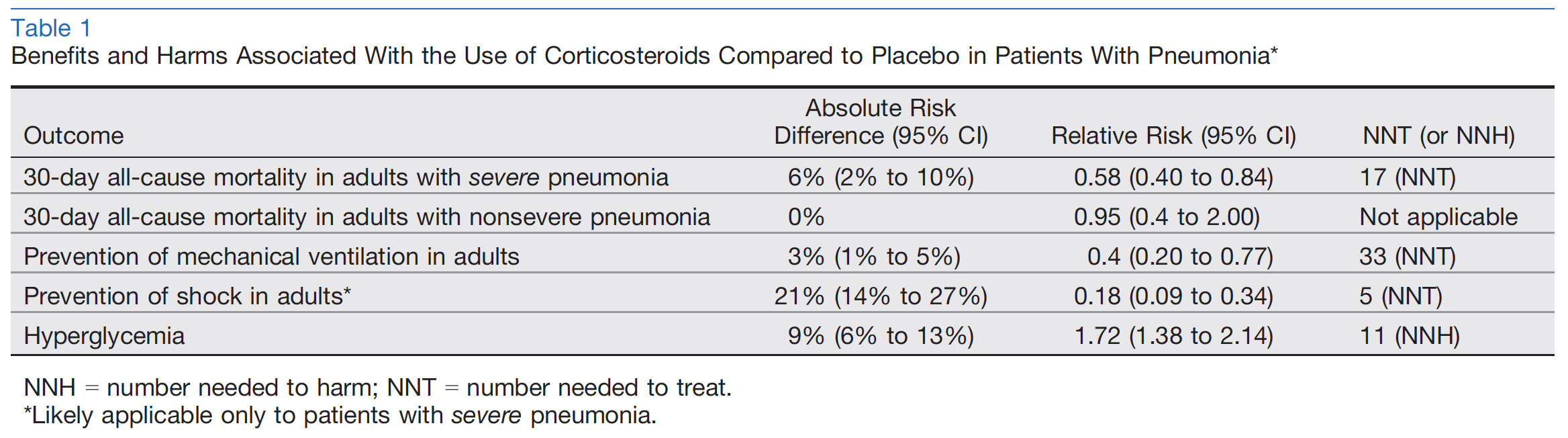
Corticosteroids, such as prednisone, play a significant role in the management of pneumonia in patients with specific conditions. They reduce inflammation and help alleviate symptoms, especially in cases of severe pneumonia or pneumonia associated with chronic respiratory diseases like COPD. Clinical studies indicate that corticosteroids can shorten recovery time and lower mortality rates in patients presenting with acute respiratory distress syndrome (ARDS) related to pneumonia.
Indications for Use
Consider corticosteroid therapy when managing pneumonia in individuals with severe disease, those requiring hospitalization, or patients with significant inflammatory responses. Guidelines recommend initiating corticosteroids for patients showing rapid deterioration, those with respiratory failure, or those requiring mechanical ventilation due to pneumonia-associated complications. The dosage and duration depend on the clinical scenario, with lower doses generally used for a brief period to minimize potential side effects.
Potential Risks and Benefits
While corticosteroids offer numerous benefits, weighing the potential risks is crucial. They can lead to increased blood sugar levels and a higher risk of secondary infections, particularly in patients with underlying health conditions. Clinicians must assess each patient’s individual health status and potential for adverse effects carefully. Monitoring during treatment ensures timely adjustments if complications arise.
Indications for Prescribing Prednisone in Pneumonia
Prednisone is indicated for pneumonia in specific clinical situations. It is most beneficial in patients with acute exacerbations of chronic obstructive pulmonary disease (COPD) or asthma, where inflammation plays a significant role. The use of prednisone in these cases aids in reducing airway inflammation and improving respiratory function.
Severe pneumonia, particularly in patients requiring hospitalization, may warrant corticosteroid therapy. This approach can help mitigate the inflammatory response that often accompanies pneumonia. It is particularly relevant for patients diagnosed with pneumonia who present with significant respiratory distress, elevated inflammatory markers, or those who are at risk of acute respiratory failure.
Specific Populations for Prednisone Use
Certain populations may benefit more from prednisone treatment:
- Patients with community-acquired pneumonia experiencing severe symptoms.
- Individuals with underlying lung diseases, such as asthma or interstitial lung disease, exacerbated by pneumonia.
- Patients requiring intensive care unit admission due to pneumonia-related complications.
Clinical Considerations
Before prescribing prednisone, consider the following:
| Factor | Consideration |
|---|---|
| Severity of Symptoms | Assess if the patient exhibits severe respiratory symptoms indicating inflammation. |
| Duration of Symptoms | Evaluation should include how long the patient has had symptoms, as prolonged symptoms may signal the need for corticosteroids. |
| Risk of Complications | Consider the patient’s risk for respiratory failure based on comorbidities and clinical presentation. |
| Response to Initial Treatment | Monitor the patient’s response to initial antibiotic therapy; lack of improvement may necessitate corticosteroid introduction. |
Use prednisone judiciously, evaluating the balance between benefit and potential adverse effects, particularly in older adults or those with comorbid conditions. Regular monitoring throughout treatment is crucial to achieving optimal outcomes.
Dosage Guidelines for Prednisone Use in Pneumonia
The typical dosage of prednisone for pneumonia ranges from 20 mg to 60 mg per day. Start with a higher dose, especially in moderate to severe cases. In cases of acute exacerbations, a higher initial dose can help reduce inflammation quicker.
For adults, a common regimen is 40 mg daily, administered in one or two doses. Reduce the dose gradually based on clinical improvement, typically tapering by 5 mg every 3-7 days. This tapering minimizes withdrawal symptoms and helps the body adjust.
For patients with severe pneumonia or those requiring hospitalization, higher doses such as 60 mg per day may be appropriate initially. Monitor the patient’s response and adjust the dosage accordingly.
In children, dosing is often based on weight, with recommendations typically at 1-2 mg/kg per day. Max doses should not exceed 60 mg per day. Adjust based on clinical response and potential side effects.
Always use caution with patients who have comorbidities like diabetes, hypertension, or gastrointestinal issues. Regular monitoring is necessary to ensure that any side effects are managed promptly. If significant side effects occur or if pneumonia symptoms worsen, reassess the need for continued steroid therapy.
Consult a healthcare professional for personalized dosing recommendations, considering the patient’s specific health needs and response to treatment.
Potential Side Effects and Risks of Prednisone
Prednisone may offer significant benefits for treating pneumonia, but it’s crucial to be aware of its potential side effects and risks. Users often experience elevated blood sugar levels, which can lead to complications, especially in diabetic patients. Regular monitoring is advisable.
Insomnia and mood changes, such as irritability or anxiety, are common during treatment. Strategies to manage these effects include establishing a regular sleep schedule and engaging in calming activities. Patients should communicate any significant mood swings to their healthcare provider promptly.
Physical Side Effects
Weight gain can occur due to increased appetite and fluid retention. Maintaining a balanced diet and regular exercise can help manage this side effect. Additionally, long-term use may lead to thinning skin and increased susceptibility to bruising. Protective measures like moisturizing and avoiding harsh products can mitigate some skin issues.
Serious Risks
Long-term prednisone therapy carries risks such as osteoporosis and increased chances of infections. Routine bone density assessments are recommended, alongside calcium and vitamin D supplementation. It’s essential to seek immediate medical attention for symptoms like severe headache or vision changes, which may indicate serious complications.
Clinical Studies and Evidence Supporting Prednisone Efficacy
Prednisone has demonstrated significant benefits in treating pneumonia, particularly in patients with severe cases or underlying respiratory conditions. A study published in the *New England Journal of Medicine* examined the use of corticosteroids in patients with COVID-19 pneumonia, revealing that those treated with prednisone had a lower risk of respiratory failure and death compared to the control group.
Clinical Trial Data
In a randomized controlled trial involving patients diagnosed with pneumonia, the administration of prednisone led to a noticeable reduction in hospitalization duration. Participants who received prednisone experienced a median recovery time that was three days shorter than those who did not receive corticosteroids. Additionally, a meta-analysis of multiple studies indicated that corticosteroid therapy, including prednisone, significantly decreases mortality rates in patients suffering from severe pneumonia.
Mechanism of Action
Prednisone works by reducing inflammation within the lungs, which aids in alleviating symptoms and promoting recovery. Research shows that the dampening of the inflammatory response allows for improved lung function, enabling faster healing. Evidence suggests that patients with pneumonia and high inflammatory markers benefited the most from prednisone, as it directly targets the immune response exacerbating their condition.
In conclusion, clinical studies consistently support the use of prednisone as a therapeutic option in pneumonia treatment, particularly for severe cases. Physicians are encouraged to consider this treatment to enhance recovery outcomes for affected patients.